New definitions in NFPA 70
There are new definitions in Article 517 of NFPA 70 that have design implications that need to be considered by the consulting-specifying engineer.
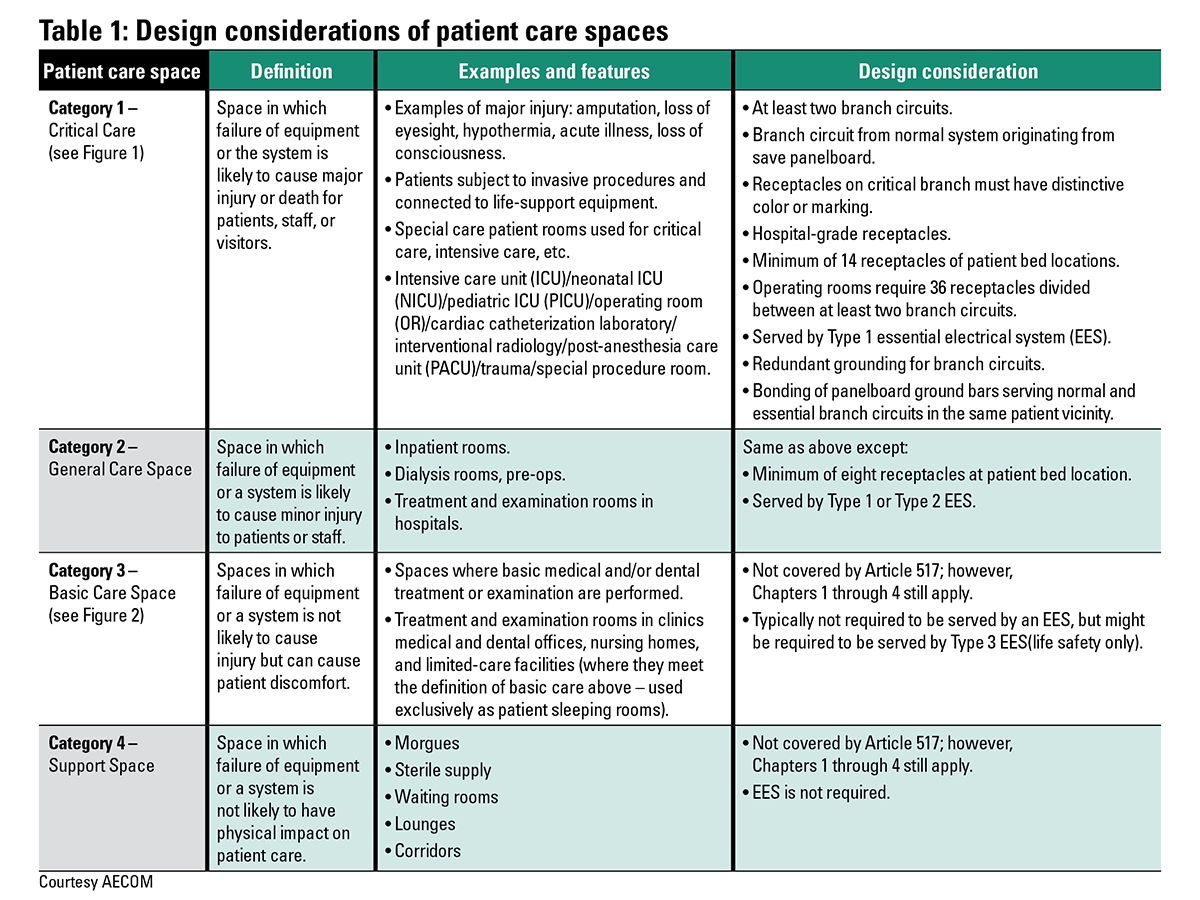
The governing body of the health care facility is “the person/s who has the overall legal responsibility for the operation of a health care facility.” The governing body establishes and identifies the patient care space categories in the health care facility based on the anticipated level of patient care and designates wet-procedure locations. The above areas of responsibility have many requirements that must be considered by the consulting engineer, including the number and type of receptacles and number of branch circuits in patient spaces, special protection against electric shock in wet-procedure locations, and loading on the alternate power source.
An invasive procedure is defined as “any procedure that penetrates the protective surfaces of a patient’s body and that is performed with an aseptic field (procedural site).” Not included in this category are special procedures such as the placement of peripheral intravenous needles or catheters used to administer fluids or medications, insertion of urethral catheters, and other similar procedures. What is important for the consulting engineer to understand about invasive procedures are what make certain spaces in a health care facility a Category 1 risk space. Category 1 spaces have special requirements in wiring, protection, and the type of the essential electrical system (EES) that supplies these spaces. NFPA 99 (Item A.6.7.5.1.3) recommends an automatic battery-operated lighting unit or system to provide minimal task illumination in invasive-procedure spaces.
A medical office is “a building or part thereof where the following occur: 1) examinations and minor treatments or procedures performed under the continuous supervision of a medical or dental professional; 2) only sedation or local anesthesia is involved and treatment or procedures do not render patients incapable of self-preservation under emergency conditions; and 3) overnight stays for patients or 24-hour operation are not provided.” What is important for the consulting engineer to understand is that there is a difference between a health care occupancy and a health care facility. All health care occupancies are health care facilities, but the opposite is not true. A health care occupancy is used to provide medical or other treatment or care simultaneously to four or more patients on an inpatient basis, where such patients are mostly incapable of self-preservation due to age, physical or mental disability, or because of security measures not under the occupant’s control. A hospital, for example, is a health care facility but can be of several different occupancies (health care, business, assembly, ambulatory, etc.). A medical office is a health care facility, but under NFPA 101 it would typically be a business occupancy.
Patient care spaces as defined in NFPA 70 are now aligned with the same definition in NFPA 99. A patient care space is “any space of a health care facility wherein patients are intended to be examined or treated.” There are four categories in health care facilities identified by the governing body based on 1) the anticipated level of patient care in any given space; and 2) the risk to the patient from procedures that will be performed.
NFPA 70-2017 “Type” classification
The 2017 version of NFPA 70 has now aligned the Type classification of the EES with NFPA 99. Type 1 and Type 2 EES are referenced in NFPA 70 Article 517.29 (Essential Electrical System Requirements for Hospitals and Other Health Care Facilities) and in Article 517.40 (Essential Electrical Systems for Nursing Homes and Limited Care Facilities), respectively. It is to be noted that the “type” terminology is also mentioned in NFPA 110 and applies to the emergency power supply system. The following paragraphs clarify what the type means as referenced in NFPA 70, NFPA 99, and NFPA 110.
NFPA 99, Item 6.7.1.2.4.1, requires that Type 1 and Type 2 EES power sources be classified as Type 10, Level 1 generator Class X, per NFPA 110. The type in NFPA 110 is the maximum time in seconds that the emergency power supply system (EPSS) will permit the load terminals of the transfer switches to be without power. The class in NFPA 110 is the maximum time in hours for which the EPSS is designed to operate at its rated load without being refueled. This means that power must be restored within 10 seconds, but the amount of time the EPSS is required to run without refueling is not defined in NFPA 110 and needs to be specified as required by other codes or by the authority having jurisdiction.
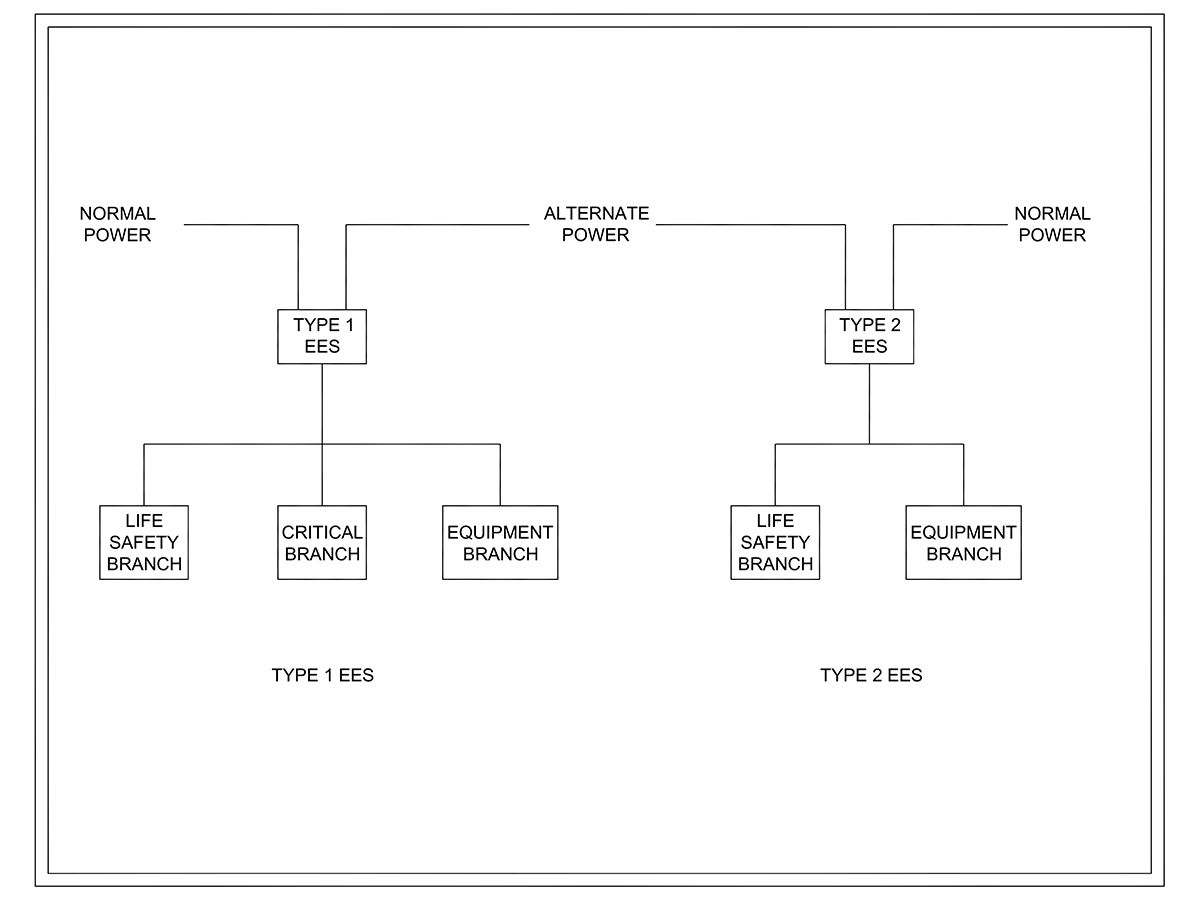
Type 1 EES per NFPA 99 and NFPA 70 consists of three branches: life safety, critical, and equipment. Type 2 EES has two branches only: life safety and equipment. Type 2 EES does not have a critical branch. The critical branch in a Type 1 EES is intended to serve loads that, if they were without power, their failure could result in death or serious injuries. See Figure 5.
Type 1 EES applies to critical care (Category 1) and general-care (Category 2) spaces in hospitals and other health care facilities where patients are sustained by electrical life support equipment. Type 2 EES applies to nursing homes and limited-care facilities. For freestanding buildings where admitting and discharging policies preclude providing care for patients who may need electrical life support equipment, or where no surgical treatment requiring general anesthesia is offered, an automatic battery-operated system would suffice to provide 1½ hours of backup lighting for exit lights, exit corridors, stairways, nursing stations, medical preparation rooms, boiler rooms, and communication areas, in addition to backup power to operate all alarm systems.
Item 517.45 clarified the type of EES required for other health care facilities (other than hospitals, nursing homes, and limited-care facilities). If electrical life support is required or if there are critical care (Category 1) spaces, then a Type 1 EES shall be provided. If there are general-care (Category 2) spaces, then a Type 2 EES is required. However, if required by the governing body of the facility, an EES is permitted and is comprised of an alternate power system capable of supplying a limited amount of lighting and power for the orderly cessation of procedures during the time normal power is interrupted.
It is to be noted that Type 3 EES has been eliminated from the 2015 version of NFPA 99 because Category 3 and 4 spaces are not required to be fed by an EES. This means that no spaces in the health care facility were required to be served from a Type 3 EES. Facilities that had previously required a Type 3 EES typically provided the type of patient care in which, if normal power was interrupted, there was a minimal risk to patients or staff. Such a facility could safely terminate procedures and basically close for business. A Type 3 EES was only required to provide 1½ hours of backup power, which is consistent with NFPA 101. It is not intended that these facilities no longer need backup power, but rather the other codes and standards or the governing body will specify limited requirements needed for safe egress from such facilities.
NFPA 70 and NFPA 99 prohibit the use of isolated ground receptacles inside of a patient care vicinity. A patient care vicinity is a space within a location intended for the examination and treatment of patients, extending 6 ft beyond the normal location of the patient bed/table and extending vertically 7.5 ft above the floor. Isolated ground refers to devices that have a ground connection, but that ground connection is derived from the building entrance rather than being directly grounded to the enclosure. Examples of where an isolated ground application might be required include diagnostic and treatment equipment that may require a dedicated or isolated ground separate from the facility’s grounding system to reduce noise when serving sensitive electronic or medical equipment. The consideration for the consulting-specifying engineer is that isolated ground is not permitted within a patient care vicinity, but it can be provided outside the patient care vicinity area.
There are other changes in the 2017 NFPA 70 outside of Article 517 that impact all types of building occupancies, but the following should especially be considered for health care facilities.
Additional arc flash energy-reduction measures have been introduced in Item 240.87, namely using circuit breakers with instantaneous trip settings that are less than the available arcing current or with an instantaneous override that is less than available arcing current. Although on one hand, instantaneous tripping would reduce arc flash energy—as arc flash energy is a function of protective device fault-clearing time and tripping current— instantaneous tripping will not allow proper circuit breaker selective coordination. The concept of selective coordination is to delay, not to instantaneously trip upstream circuit breakers to allow downstream breakers localized to the fault to trip first. Consulting-specifying engineers should conduct an overcurrent protective study and balance the trade-off between lower arc flash energy and circuit breaker selective coordination.
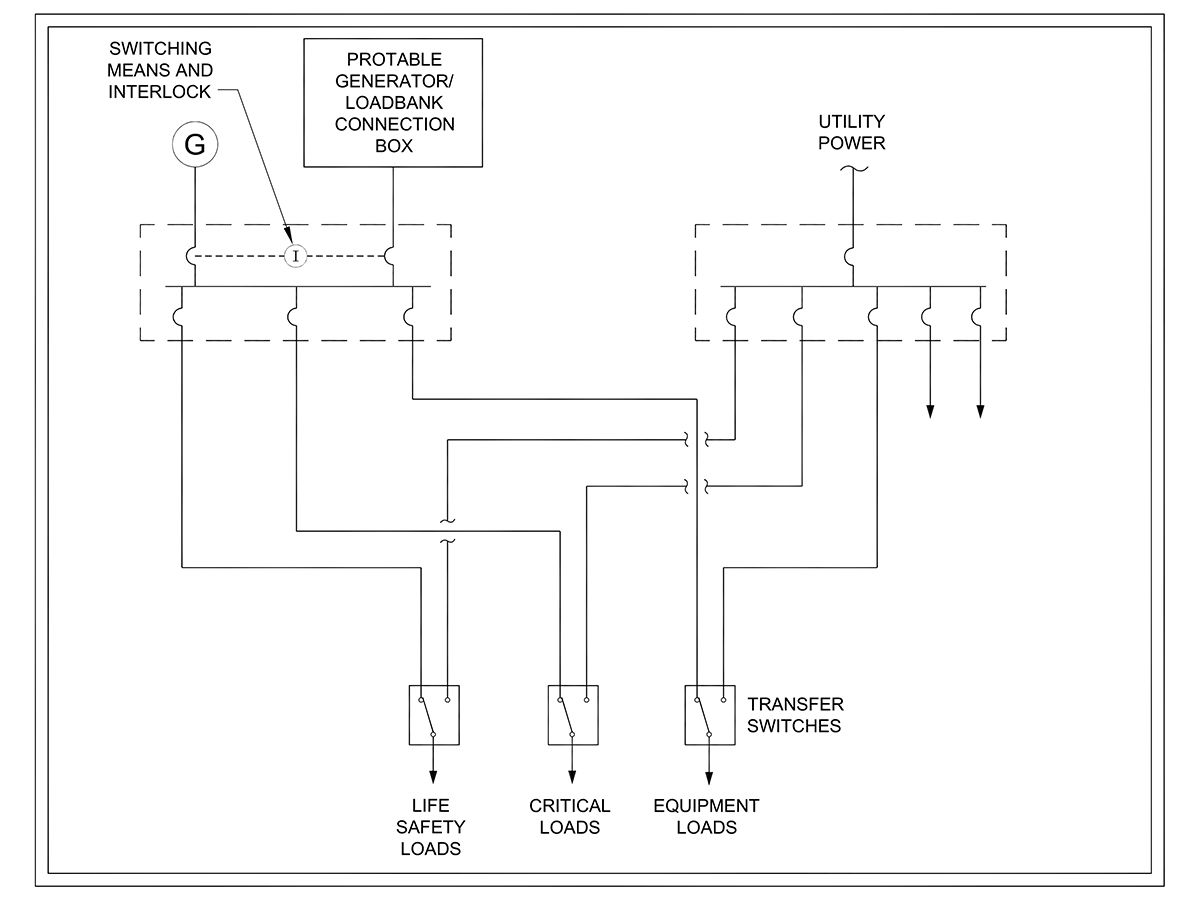
There are also notable changes in NFPA 70-2017 made to Article 700. Article 700.3.F now calls for an emergency system that relies on a single alternate source of power that will be disabled for maintenance or repair, to include a permanent switching means to connect a portable or temporary source of power, and be available for the duration of the downtime. Manual switching is allowed to be used in this case to switch from the permanent source to the portable source. Some health care facilities have multiple alternate power sources, such as generators connected in an N or N+1 configuration. In a two-generator scheme connected in parallel in N configuration and supplying 100% of the total essential load, either generator would comply with the above requirement in this case, if it can support the life safety system load by itself. The portable or temporary power-source connection could also be used to connect a portable load bank to comply with NFPA 110 periodic maintenance testing and loading requirements, which are mandatory for Level 1 and Level 2 standby and emergency power systems. See Figure 6.
Another important requirement that has been added in NFPA 70 Article 700.10(D)(3) is fire protection for emergency (life safety) feeder circuit wiring for health care occupancies where patients are not capable of self-preservation, such as hospitals and ambulatory care occupancies. The code lists a number of options to comply with this requirement including installing life safety feeders in spaces that are protected by an approved fire-suppression system, using feeder cables that are a listed electrical circuit protective system, or encased in a minimum of 2 in. of concrete. As required by other codes, a water-based sprinkler system is typically provided in health care occupancies; however, the code stipulates that running feeders above a ceiling in an otherwise fully sprinklered building does not meet the requirement unless there are also sprinklers in the plenum space above the ceiling. Without proper consideration to the routing of feeders, this new requirement could have a very large financial impact on the installation. The consulting engineer might consider installing emergency feeders in areas that are typically fully sprinklered, such as vertically within electrical rooms or horizontally in areas without a suspended ceiling, and avoiding horizontal feeder runs above suspended ceilings that are not sprinklered, to avoid the additional cost of the other fire protection measures.
Another addition to Article 700 of NFPA 70 which is directly related to Article 517, is a new requirement for generator-control wiring. The article states that generator-control wiring installed between the transfer equipment and the emergency generators must be kept entirely independent of all other wiring and must be protected against fire in line with the fire protection measures listed above. Article 700.10(D) (3) now calls for continuous monitoring of the integrity of the generator-control wiring. Without this monitoring, an open circuit on the control wiring would go undetected and won’t be noticed until there is a power outage and the generator fails to start. This new requirement entails three elements: 1) continuous monitoring of generator signal circuits; 2) visual and audible annunciation; and 3) automatic transmission of an engine start signal and an alarm when a problem is detected. Several transfer switch manufacturers offer an easy solution for existing and new installations. Existing wiring does not need to be changed in this case, but additional circuit-communication modules would have to be added at both ends of the control wiring: at the generator and at the transfer equipment.
Article 517 of NFPA 70 has many design considerations for the consulting engineer designing health care facilities. These design considerations cover the wiring and protection of the electrical distribution system in patient care spaces and the EES in various health care occupancies.
Firas (Ross) Alkhayri, PE, CEM; AECOM, Columbus, Ohio
Author Bio: Firas (Ross) Alkhayri is the electrical department manager at AECOM's Columbus, Ohio, office. He has more than 25 years of experience in the design of power and emergency systems for a wide variety of mission critical facilities.